As many as 25-45% of women experience urinary incontinence at least once a year. While older women are more likely to experience urinary incontinence, young and middle-aged women are also affected by this problem. Yet, many of these women believe that this is a normal part of aging or a consequence of giving birth. Because of this, many women don’t seek treatment for their symptoms since they don’t realize what is normal and what is not. Therefore, it is important to evaluate what is normal and what is not normal in order to determine if you could benefit from treatment.
What is normal?
On average your bladder can hold around two cups of urine, which means that you will need to empty your bladder about 5-7 times during a 24 hour period. In older women, it is normal to urinate more frequently as bladder capacity decreases. This usually means that older women urinate about 8 times during the day and may wake once during the night to urinate.
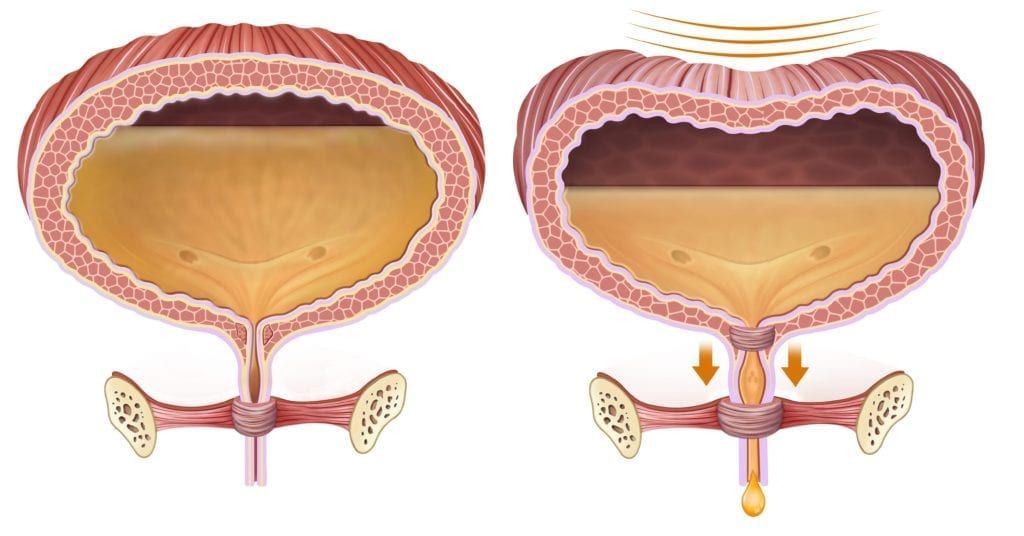
As the bladder begins to stretch and fill with liquid, it is normal to experience the urge to urinate. However, urges are felt before the bladder is completely full and should be able to be controlled. Once urination begins, it is normal for urine to flow steadily without exertion or discomfort until the bladder has been emptied.
What is not normal?
Now that we have taken a closer look at what is normal for your bladder, let’s look at some abnormalities:
- Frequent feelings of urgency followed by an inability to get to a bathroom in time (usually a few seconds or a few minutes warning)
- Inability to urinate despite feeling the urge to urinate
- Weak stream of urine or a stream that starts and stops
- Feeling like you cannot empty your bladder completely
- Experiencing a constant dribble of urine
What to do if you are experiencing symptoms:
In looking at what is normal and what is not normal for your bladder, you may have realized that you have been experiencing symptoms of urinary incontinence. Luckily, there are a variety of treatments available to manage your symptoms. The first step is to schedule an appointment with a urogynecologist to discuss your symptoms and receive a personalized treatment plan.
During your appointment, your urogynecologist will ask you to provide information about your medical history (including childbirths, procedures, surgeries, illnesses, or injuries), current health problems and medications, and whether you’ve ever had problems with your urinary system before. They will use this information to determine your individual treatment plan.
Although treatment plans can vary among the individual, some general guidelines may include:

- Avoid drinking large amounts of liquids at once and instead drink small amounts somewhat frequently
- Drink at least 6 cups of fluid daily
- Limit or avoid caffeine, alcohol, carbonated drinks, and acidic foods/beverages
- Quit smoking
- Eat a high fiber diet to avoid constipation
- Practice exercising your pelvic floor muscles (Kegels)
In addition to these guidelines, your urogynecologist may also recommend other forms of treatment such as bladder training, electrical stimulation, estrogen creams, implants, medications to reduce feelings of urgency, or surgery. However, surgery is generally performed as a last resort option after a variety of conservative methods have failed.

Dr. Geoffrey Zann is a Certified Robotic Da Vinci Surgeon, Board-certified by the American College of Obstetricians and Gynecologists, and a Diplomat of the American Board Obstetrics of Gynecology. He has been a member of the American Society for Colposcopy and Cervical Pathology, American Association of Gynecologic Laparoscopists, and the Hugh R. K. Barber Obstetric and Gynecologic Society.