Uterine prolapse is a common condition that affects women, especially those over the age of 50. It is characterized by the uterus falling toward or into the vagina as a result of weak pelvic floor muscles and ligaments. It can be caused by things like pregnancy, vaginal delivery, menopause, and frequent straining. Although many women are hesitant to talk with their doctors about this condition, it is easily treatable with both non-surgical and surgical options.
Uterine prolapse can either be incomplete or complete. Incomplete uterine prolapse describes when the uterus is partially displaced in the vagina, but does not protrude. Complete uterine prolapse describes when the uterus is completely displaced in the vagina, with part of the uterus protruding from the vaginal opening.
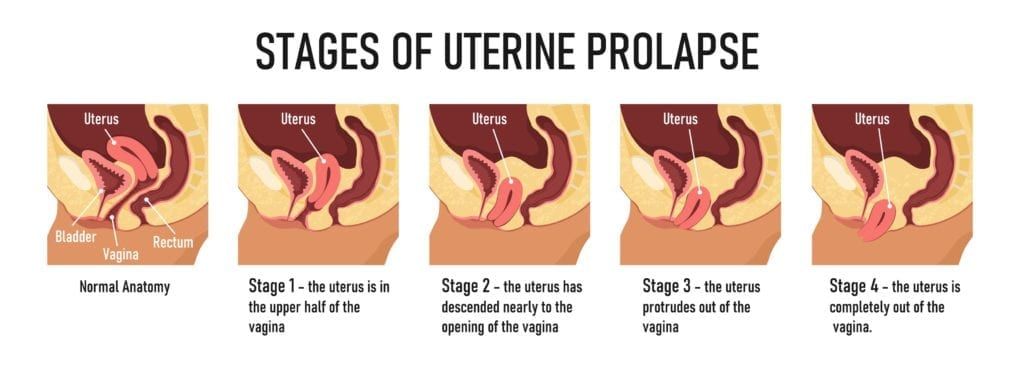
In addition to being characterized as incomplete or complete, uterine prolapse is also categorized by the severity of the descent. There are four grades used to describe the severity of the uterus’ descent.
- 1st grade: uterus has descended into the upper vagina
- 2nd grade: uterus has descended into the introitus (vaginal canal)
- 3rd grade: cervix has descended out of the introitus
- 4th grade: uterus and cervix have descended out of the introitus
In the early stages of uterine prolapse, you may not experience any symptoms, or you may experience them intermittently and may notice they get worse at night. Generally speaking, the more the condition progresses, the number and severity of symptoms is expected to increase. Some symptoms of uterine prolapse include:
- A feeling of heaviness or pulling in the pelvis
- Lower back pain
- Urinary problems
- Sensations that something is falling out of the vagina
- Pain during sex
To diagnose uterine prolapse, your gynecologist will ask you about any symptoms you have been experiencing. Then they will perform a physical examination to determine organ placement and vaginal elasticity. In some cases, additional imaging techniques, such as an ultrasound or MRI, may be used to determine the grade of the prolapse.
Once the severity of the prolapse has been determined, your gynecologist will discuss your treatment options. In general, milder cases can usually be treated with non-surgical treatments such as kegels, estrogen therapy, maintaining a healthy weight, and avoiding behaviors that cause straining. More severe cases, as well as cases that continue to progress, may be best treated with surgical intervention. However, women who are intending to get pregnant in the future are not ideal candidates for surgery. Ultimately, since every case is different your gynecologist can help you decide which treatment option is best.
In the case that surgery is recommended, there are different surgical options that can be used. One option is uterine suspension, where the pelvic ligaments are properly reattached or reinforced with medical materials. By repairing the ligaments, this surgical approach places the uterus back in its proper position. Nowadays, uterine suspension surgery can easily be performed as a minimally invasive surgery with tiny incisions, little to no hospital stay, and a faster, less painful recovery.
Another surgical option to treat uterine prolapse is to have a hysterectomy, which is a surgical procedure that removes the entire uterus from the abdomen. In some cases, the ovaries and fallopian tubes will also be removed during a hysterectomy. Since a hysterectomy is a permanent form of sterilization, this approach is generally only recommended for post-menopausal women.
Overall, uterine prolapse is a common condition that affects women and can easily be treated with non-surgical and surgical procedures. Mild cases, as well as some more severe cases, tend to respond well to non-surgical treatment, however there are still cases where surgical treatment may be recommended. Ultimately, only your gynecologist can tell you if surgery is the right option for your individual case of uterine prolapse.

Dr. Geoffrey Zann is a Certified Robotic Da Vinci Surgeon, Board-certified by the American College of Obstetricians and Gynecologists, and a Diplomat of the American Board Obstetrics of Gynecology. He has been a member of the American Society for Colposcopy and Cervical Pathology, American Association of Gynecologic Laparoscopists, and the Hugh R. K. Barber Obstetric and Gynecologic Society.