Did you know that women are twice as likely as men to experience urinary incontinence? Although many women who experience urinary incontinence are ashamed to talk about it, this problem is highly common, especially in women who have had multiple vaginal deliveries. Contrary to popular belief, urinary incontinence in women is not a result of aging and there are treatment options available to resolve the issue.
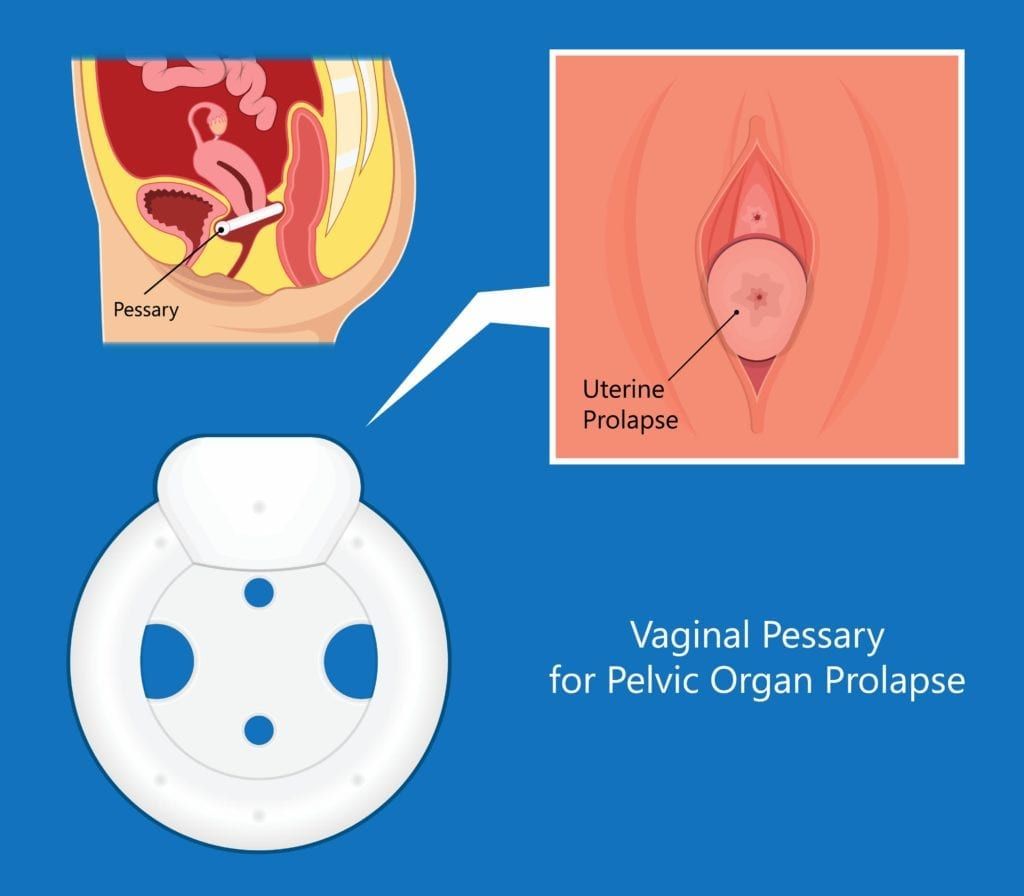
One treatment for urinary incontinence is known as a pessary, which is a soft, removable device made of silicone that fits inside the vagina and under the cervix in order to provide additional support. It is commonly used to support the bladder, uterus, vagina, small bowel, and rectum, which are all organs affected by pelvic floor disorders. Pelvic floor disorders occur when the pelvic floor muscles have been placed under increased pressure in the abdomen. The most common cause is pregnancy, labor, and childbirth, however obesity and genetics can also play a role.
Urinary incontinence is one of the most common symptoms of a pelvic floor disorder, as well as one of the symptoms that a pessary can treat. Depending on the severity of the prolapse, there are different types of pessaries that your gynecologist may recommend, including:
- Ring: like its name suggests, a ring pessary is a circular ring that you can easily place on your own. Since it is so easy to place, this is generally the type of pessary your doctor will recommend starting with
- Gehrung: this type of pessary is customized to fit its user and is recommended for more advanced uterine prolapse
- Gellhorn: this type of pessary is round with a small knob in the middle which provides additional support for cases of severe prolapse
- Cube: this type of pessary uses suction to remain in place and provide support. It is used for extremely severe prolapse cases
Since there are different types of pessaries, your gynecologist will perform a vaginal exam to determine the severity of your prolapse. They will also take measurements to determine the best size so that the pessary does not fall out or cause discomfort. When having a pessary placed, your gynecologist may try different styles and sizes to determine the right fit. After finding the best fit, your gynecologist will show you how to place and remove your pessary, as well as how to clean it.
You can also expect to have regular follow up appointments with your gynecologist so that they can continue to monitor your condition and determine if the pessary is working properly. After the initial placement, your doctor will have you come back in a week to make sure there is no vaginal irritation or problems with the fit. Then you will usually have follow ups at the two week and six month mark, unless otherwise directed by your gynecologist.
In between appointments, you will need to care for your pessary by removing and cleaning it. On average, you should remove your pessary every night or every week to clean it with mild soap and water before reinserting it in your vagina. However, certain pessaries, such as the Gellhorn, can only be safely removed by your gynecologist. In these cases, you will schedule regular appointments every 1-3 months in order to have the pessary removed and cleaned.
Overall, pessaries are silicone devices that are placed inside the vagina under the cervix to help provide support to the surrounding structures affected by pelvic floor disorders. This additional support can decrease or eliminate symptoms associated with pelvic floor disorders, such as urinary incontinence in women. If you have been struggling with urinary incontinence, it’s time to speak up and make an appointment with your gynecologist to be fit for a pessary.

Dr. Geoffrey Zann is a Certified Robotic Da Vinci Surgeon, Board-certified by the American College of Obstetricians and Gynecologists, and a Diplomat of the American Board Obstetrics of Gynecology. He has been a member of the American Society for Colposcopy and Cervical Pathology, American Association of Gynecologic Laparoscopists, and the Hugh R. K. Barber Obstetric and Gynecologic Society.